
Health Care
Medicaid spending, enrollment escalated during shutdowns
November 11, 2020
Kaitlyn Finley
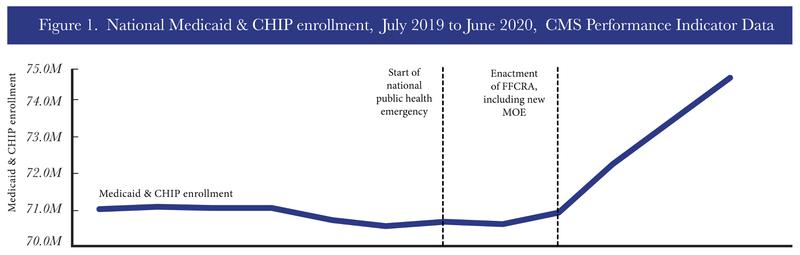
Due to economic fallout from the coronavirus beginning in March, Medicaid enrollment spiked nationally by 4 million—up to 74.6 million by June, according to the latest data from the Centers for Medicare and Medicaid Services. (The chart below includes the Children’s Health Insurance Program (CHIP), which provides Medicaid benefits to certain low-income children whose parents make too much to qualify for Medicaid.)
In response to the government-imposed coronavirus lockdowns, Congress passed the Families First Coronavirus Response Act (FFCRA) in March to increase the amount of funding available to states for its Medicaid programs. A recent report from the Congressional Budget Office projected the additional funding for Medicaid this year will increase federal spending by $41 billion this year and $132 billion from 2021-2030.
Before the pandemic, Medicaid outlays were already set to rise dramatically, in part due to expanding Medicaid benefits to able-bodied adults.
Since the implementation of Obamacare in 2013, total annual taxpayer dollars spent on Medicaid have dramatically increased and are on pace to hit $1 trillion in five years according to the U.S. Department of Health and Human Services.
Before Obamacare, free and low-cost health care benefits under Medicaid were only extended to those who could not secure gainful employment, such as children, low-income pregnant women, low-income caretakers, or those with disabilities. But Obamacare expanded Medicaid coverage to able-bodied adults who make less than $36,156 annually in a four-person family.
According to the MACPAC, the Congressional Commission that tracks Medicaid data, nearly 15 million adults have enrolled in Medicaid under expansion from 2013 to 2018. The federal government and states that have opted to expand Medicaid have collectively spent $303 billion on Medicaid expansion from 2014 to 2018. (Source: 2016, 2017, and 2018 U.S. Department of Health and Human Services Actuarial Report on the Financial Outlook for Medicaid)
Data from the National Association of State Budget Officers show Medicaid accounts, on average, for nearly 29 percent of all state spending. States are having to raise revenue in order to pay for increased costs associated with expansion. Last year the Washington Post reported that expansion forced 13 states to raise taxes or fees to keep budgets afloat. As states begin to recover from lost economic production and revenue due to the coronavirus, it is crucial that states conduct proper audits of their growing Medicaid programs and ensure only those eligible receive services.